Case history 7
CASE HISTORY 7
Blood sugar random
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
A 45 years old male patient presented to the opd with chief complaints of :
fever with chills since 4 days
HISTORY OF PRESENT ILLNESS:
patient is apparently well 4 days back with his daily work like farming and then he developed fever with chills where he cannot do his work he went the near by hospital and given medication subsided temporarily and suggested to a big hospital for further treatment .
He also complains of generalised body pains and headache
PAST HISTORY :
patient has no similar history in the past . And
No history of diabetes
No history of hypertension
No history of asthma
No history of cold
No history of cough
No history of vomiting or loose stools
PERSONAL HISTORY :
appetite : normal
Diet : normal
Bowel and bladder : normal
Micturition : normal
Addictions : takes alcohol occasionally
FAMILY HISTORY :
there are no similar complaints in the family members
TREATMENT HISTORY :
patient took medication for fever which is given by the local doctor in which the fever subsided temporarily.
GENERAL EXAMINATION :
Patient is conscious, coherent , and patient consent is taken and well oriented to time and place
And examined in a well lit room
Patient is moderately built and moderately nourished
Pallor not seen
Cyanosis not seen
Lymphadenopathy not seen
Pedal edema not seen
Icterus not seen
Clubbing not seen
VITALS :
Temperature : 98.8 ° F
Blood pressure : 130 / 90
Pulse rate : 70
Respiratory rate : 18
SPO2 : 98 % of room air
SYSTEMIC EXAMINATION :
RS : BAE is positive
CVS : S1 and S2 are heard
CNS : NAD
PA : soft and non tender
INVESTIGATIONS :
CUE :
TPR graphic sheet :
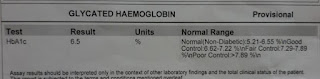
GLYCATED HEMOGLOBIN :
TREATMENT :
INJ taxim 1g iv / bd
IVF NS , RL 100 ml per hour
INJ pantop 40 mg po/ od
INJ optineuron 1 amp in 100 ml NS / IV / OD
TAB PCM 650 mg po / bd
Temperature, BP , PR , monitoring 4th hourly
Plenty of oral fluids
Strict I / o charting
PROVISIONAL DIAGNOSIS :
Viral pyrexia with thrombocytopenia











Comments
Post a Comment