Case history
CASE HISTORY 8
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan .
A 15 year old male patient presented to the opd 4 days back with chief complaints of :
Shortness of breath since yesterday
Orthopnea is present
HISTORY OF PRESENT ILLNESS :
patient was apparently asymptomatic before one month back who is studying 9 th class with a normal routine of waking up and having breakfast and going to school
and then developed fever which got subsided after taking medication
After this he developed vomitings which are usually during night time generally after taking food vomitus is usually devoid of blood and presence of food particles is seen
After consulting a near by hospital they got to know that he is suffering from kidney disease in which he got dialysis upto 10 times nearly .
Patient also complains of chest pain during shortness of breath
PAST HISTORY :
patients complains of no similar complaints in the past
Hytensive since 1 month and is on Tab . Amlong 5 mg
No h/o of diabetes .
H/ o of blood transfusions 3 times one month back
No history of asthma
No history of epilepsy
No history of thyroid disorders .
No history of any surgeries in the past
FAMILY HISTORY :
There are no similar complaints in the family members .
PERSONAL HISTORY :
Diet : mixed
Appetite: decreased
Bowel and bladder : normal
Sleep : adequate
No addictions of alcohol and smoking
TREATMENT HISTORY:
patient took medication for fever and vomitings which is given by the local hospital
And also got dialysed nearly 10 times
GENERAL EXAMINATION :
Patient consent was taken and he is cooperative, conscious , and well oriented to time and place
And he is examined under well lit room.
Pallor - seen
Icterus not seen
Clubbing not seen
Cyanosis not seen
Generalised lymphadenopathy not seen
Pedal edema not seen
Vitals :
Temperature : afebrile
Pulse rate : 96 bpm
Respiratory rate : 24 cycles /min
BP : 140/100 mm of Hg
SpO2 : 86 % at Room air .
GRBS : 121 mg%
Systemic Examination:
CVS: S1,S2 heard no murmurs
CNS: normal
RS :
Bilateral Air Entry - present
Bilateral crepitations heard at IAA and ISA.
No wheeze .
PA:
Soft ,non tender
Bowel sounds +
CNS:
NAD
PREVIOUS REPORTS :
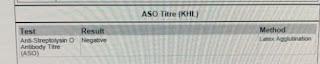
Investigations :
HEMOGRAM :
Treatment :
1. Tab Lasix 40mg po/ BID
2. Neb with duolin ,budecort -8th hourly
3.Tab .Zoffer - 4mg po /TID
4. Tab .Nodosis -500mg po /BID
5. O2 inhalation to maintain SpO2
6. Tab orofer AT po /BID
7.STRICT I/O CHARTING
8. BP ,PR,RR CHARTING
9. Tab Rantac 150 mg po /OID .
1. Tab Lasix 40mg po/ BID
2. Tab telma 20 mg po/bd
3.Tab .metxl 25 mg/PO/bd
4. Tab .nicardia 10 mg po /od
5. Fluid restriction less than 1 litre per day
6. Tab orofer AT po /BID
7.salt restriction less than 2 g per day
8. BP ,PR,RR CHARTING
9. Tab shelcal - ct po /od .



























Comments
Post a Comment